
In the fast-paced environment of an ICU, even experienced clinicians can miss critical respiratory events. One of the most under recognized — yet impactful — issues is patient-ventilator asynchrony (PVA). These mismatches between a patient's breathing effort and the ventilator's support can have serious consequences, but they're surprisingly easy to overlook.
Patient-ventilator asynchronies are common — and often undetected. In a large 2025 multicenter study of 900 ICU professionals, only 3.67% of clinicians were able to correctly identify all six types of PVAs, and over 12% failed to identify any at all [1].
This isn't a matter of skill or attentiveness — it's about data overload, lack of waveform training, and the limitations of traditional ventilator alarms.
Even with experience, detection remains inconsistent. In fact, the study showed that clinicians with years of ICU experience were no more accurate than their less experienced peers. The biggest factor that improved detection? Specific training in PVAs, which made clinicians more than twice as likely to identify all key events correctly (OR = 2.38).
What's worse: these mismatches can directly impact ventilation efficiency, patient comfort, and even clinical outcomes, leading to:
Most ICUs rely on ventilator alarms and spot checks. But alarms are blunt tools — they alert you to thresholds, not trends. And waveform analysis, while rich with insight, is rarely used in real-time because:
In practice, this means that a lot of information is left unprocessed, even though it's right there on the screen. The 2025 study also found that more than 60% of clinicians adjusted ventilation settings only once or twice during their shift, and over 10% didn't monitor waveforms at all — highlighting just how hard it is to catch these events manually.
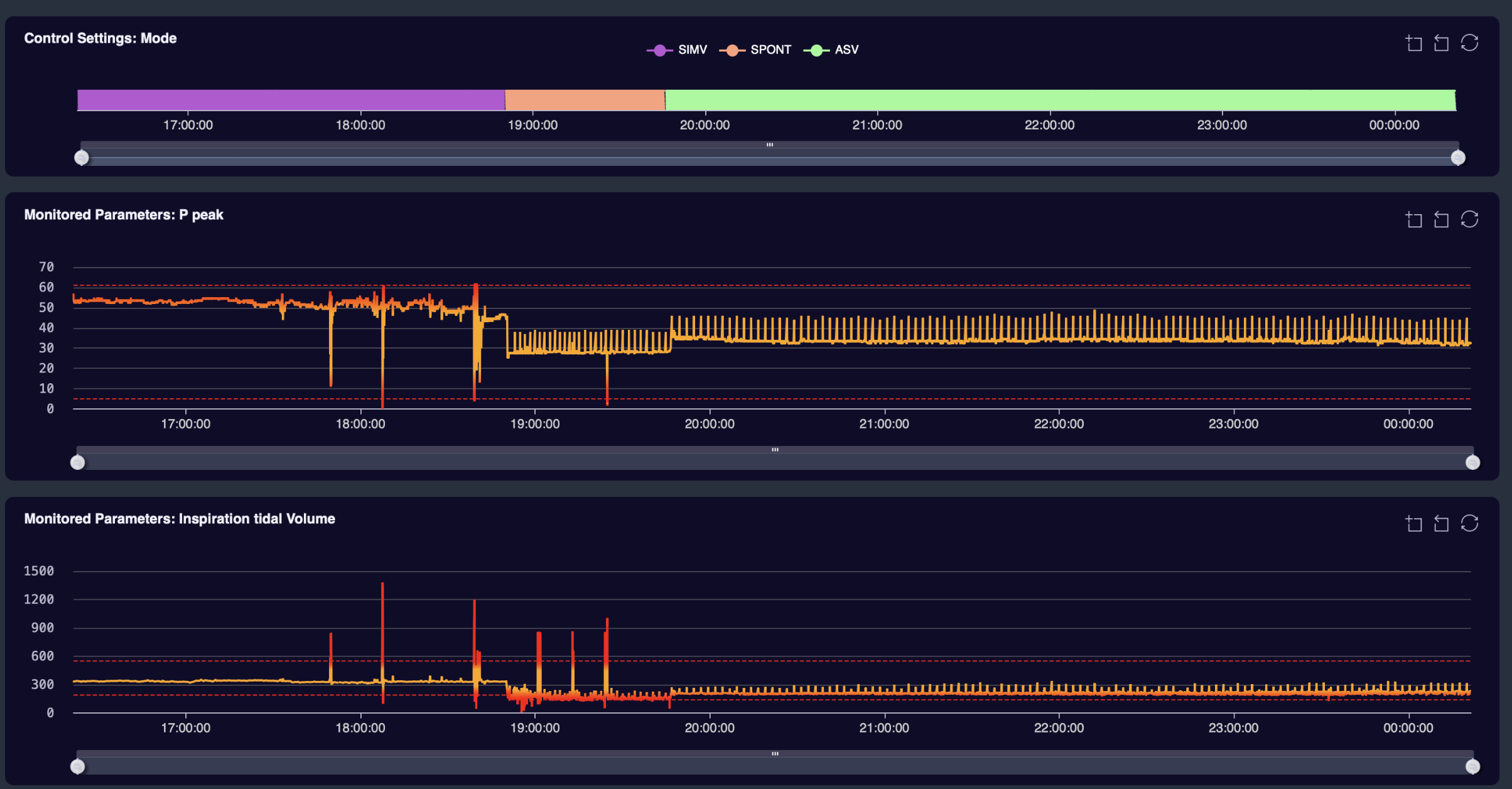
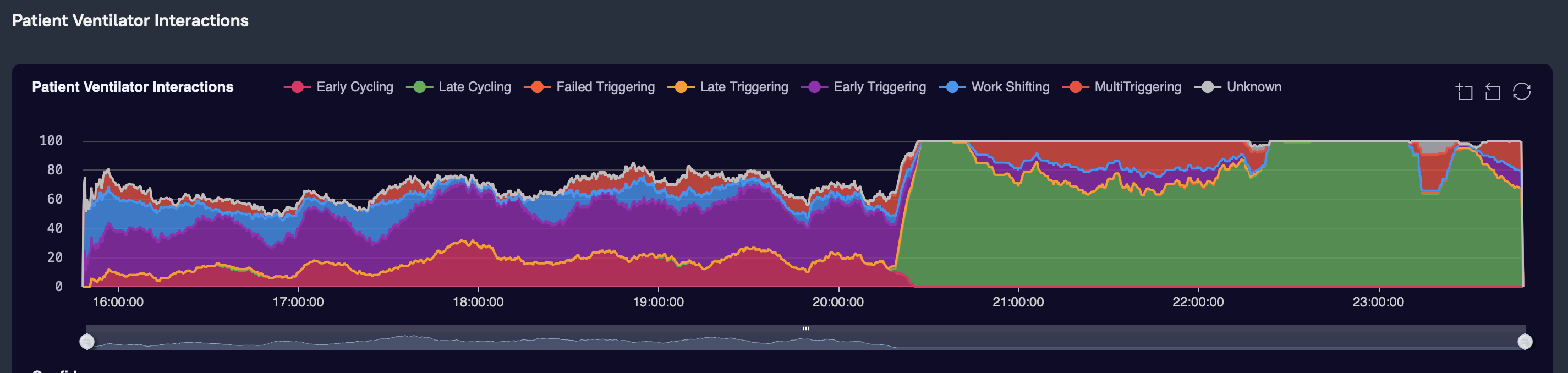
That's where AI-powered waveform analysis comes in. At Deep Breath, we built a system that continuously reads raw ventilator waveforms — the same data clinicians see on screens — but detects patterns and alerts users only when a clinically relevant asynchrony is likely happening.
Instead of another alarm, clinicians get:
Deep Breath was co-developed with ICU professionals from multiple hospitals across Europe. We prioritized ease of use and clarity over complexity. You don't need to be a data scientist to benefit — just a clinician who wants to understand what's really happening between your patient and their ventilator.
And because we analyze data in real-time, you're not waiting for end-of-shift reviews to find out what went wrong — or right.
Improving mechanical ventilation starts with seeing more — and missing less. Deep Breath is already in use across ICUs and research institutions in six countries, helping clinicians detect PVAs that would otherwise go unnoticed.
→ Want to see how it works? Book a demo or learn more
[1] Popayán A.M. et al. (2025). Ability to identify patient-ventilator asynchronies in intensive care unit professionals: A multicenter cross-sectional analytical study. The Journal of Critical Care Medicine.